Introduction: Shattering Long-Held Beliefs
For decades, spinal cord injury (SCI) represented a devastating and largely irreversible condition, leaving millions worldwide with permanent paralysis and profound life changes. Consequently, the notion of reversing such damage seemed relegated to science fiction. However, a seismic shift is occurring within regenerative medicine. Recent, credible advancements confirm that stem cell nerve therapy targeting spinal cord injuries is not merely theoretical; it is actively progressing through human clinical trials with tangible, promising results. This blog delves into the compelling evidence, the science behind it, the current state of play, and the cautiously optimistic future it heralds.
The Core Science: Harnessing Regeneration
To appreciate these breakthroughs, understanding the fundamental science is crucial. Spinal cord injuries typically involve severed or crushed nerve fibers (axons) and the loss of vital neural cells. Critically, the adult central nervous system possesses very limited innate capacity for self-repair. Stem cell therapies aim to overcome this limitation. Primarily, researchers utilize two powerful types:
- Induced Pluripotent Stem Cells (iPSCs): These are adult cells (like skin or blood cells) scientifically “reprogrammed” back to an embryonic-like state. Subsequently, they can be differentiated into virtually any cell type, including neural stem cells and specific neurons needed for spinal cord repair. Significantly, this avoids ethical concerns associated with embryonic stem cells and offers potential for patient-matched therapies.
- Neural Stem Cells (NSCs): These are progenitor cells already committed to becoming cells of the nervous system (neurons, astrocytes, oligodendrocytes). They can be derived from various sources, including fetal tissue (under strict ethical guidelines) or differentiated from iPSCs.
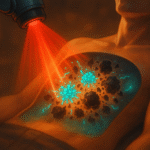
The core therapeutic strategy involves transplanting these carefully prepared stem cells into the injury site. The goal is multifaceted: to replace lost neurons and supporting cells, to secrete growth factors that foster a healing environment, to remyelinate damaged axons (restoring signal conduction), and potentially, to bridge the injury gap and regrow neural connections. Ultimately, the aim is functional restoration – movement, sensation, and autonomy.
Evidence from the Frontlines: Active Human Trials
The most compelling validation comes directly from ongoing clinical research. Multiple independent trials across the globe are reporting progress:
XellSmart’s Pioneering Global Trial (2025)
A landmark development occurred in May 2025. XellSmart, a Chinese biotech firm, secured approvals from both the US FDA and China’s NMPA for the world’s first registrational Phase I clinical trial using an allogeneic (donor-derived) iPSC therapy for SCI. This trial is particularly ambitious, aiming not just for safety but to demonstrate the therapy’s potential to actively regrow neural tissue and reverse paralysis. Its global nature underscores the seriousness of the endeavor and the level of regulatory confidence achieved[1].
UC San Diego’s Neural Stem Cell Milestone (2024)
Researchers at UC San Diego published results from their Phase I trial implanting human neural stem cells into patients with chronic spinal cord injuries (meaning the injury was not recent). Importantly, the study confirmed the procedure’s safety and feasibility. Furthermore, remarkably, two out of four patients exhibited sustained neurological improvements – including gains in motor function and sensation – observed over an extensive five-year follow-up period. Building on this success, the team is actively preparing for a Phase II trial to rigorously assess efficacy in a larger group[2][3].
Keio University’s Encouraging Results in Japan (2025)
Japanese scientists at Keio University reported treating four spinal cord injury patients with neural stem cells derived from iPSCs. While primarily focused on safety, the outcomes were highly encouraging. Crucially, no serious adverse events occurred. Moreover, two patients demonstrated improved motor function following the implantation of over two million iPS-derived cells. Notably, one individual regained the ability to stand and commenced walking practice – a monumental step forward for someone previously paralyzed[4].
Ongoing US Efforts (Mayo Clinic and Others)
Complementing these specific trials, institutions like the Mayo Clinic and others across the US continue investigating various stem cell injection approaches for SCI. Collectively, these studies have reinforced the safety profile of carefully administered stem cell therapies in this context. Additionally, they have documented variable but meaningful improvements in sensory perception and motor control among some participants, highlighting the potential while emphasizing the need for further protocol optimization[5][6].
Navigating Challenges and Complexities
Despite the undeniable progress, it is essential to temper excitement with realism. Significant scientific and logistical hurdles remain:
Optimizing Cell Type and Source
Determining whether iPSCs, NSCs, or other derivatives (like oligodendrocyte progenitors) are most effective for different injury types and locations is an active area of research. Similarly, autologous (patient’s own) vs. allogeneic (donor) cell sourcing presents distinct advantages and challenges regarding cost, time, and immune response.
Delivery and Integration
Precisely delivering cells to the optimal location within the complex and delicate spinal cord environment is technically demanding. Ensuring the transplanted cells survive, integrate functionally with the host’s existing neural circuitry, and form the correct connections is paramount and incredibly complex.
Timing of Intervention
The inflammatory environment immediately after injury differs vastly from the chronic, scarred phase. Consequently, the optimal therapeutic window and whether different cell types or support therapies (like biomaterial scaffolds or rehabilitation) are needed at different stages are critical questions.
Measuring Efficacy
Spinal cord injuries are highly heterogeneous. Therefore, designing trials with sensitive, standardized outcome measures that can reliably detect meaningful functional improvements across diverse patient populations is challenging but essential.
Scalability and Accessibility
Moving from successful trials to widely available, affordable therapies requires overcoming manufacturing complexities, ensuring consistent quality control, and navigating health system reimbursement pathways.
The Path Forward: Cautious Optimism
While acknowledging these challenges, the trajectory is undeniably positive. The combined evidence confirms that stem cell nerve therapy for spinal cord injury is a real and rapidly evolving field. The transition from promising preclinical studies to multiple concurrent human trials demonstrating both safety and preliminary signs of efficacy marks a pivotal moment in neuroscience and regenerative medicine.
Looking ahead, the focus intensifies on Phase II and eventual Phase III trials. These larger studies are designed to robustly confirm effectiveness, identify which patient populations benefit most, refine dosing and delivery protocols, and solidify long-term safety data. Simultaneously, research continues apace to enhance cell survival, integration, and functional outcomes, often combining stem cells with other supportive technologies.
Conclusion: A Transformative Dawn
In conclusion, the question “Is stem cell nerve therapy for spinal cord injury real?” receives a resounding and evidence-based affirmation: Yes. The landscape has fundamentally changed. No longer confined to laboratories or animal models, these therapies are actively being evaluated in human patients across the globe. Early results, while not yet constituting a universal cure, offer something profoundly valuable: tangible hope and demonstrable progress.
Patients who participated in these trials and experienced improvements in sensation, movement, or even regained abilities like standing, represent living proof of concept. Their outcomes, coupled with the rigorous scientific pursuit documented in these trials, signal that the long-held dream of reversing paralysis is inching towards reality. Undoubtedly, challenges persist, and widespread clinical availability may still be years away. Nevertheless, the collective advancements by institutions like XellSmart, UC San Diego, Keio University, Mayo Clinic, and others illuminate a path forward that was unimaginable just a generation ago. Stem cell nerve therapy has moved definitively beyond hope and into the realm of promising, active reality for spinal cord injury repair. The future of regenerative neurology has never looked brighter.